By Ward Dean, M.D.
This is the first of a two-part series about common health problems of women, and how, in clinical trials, natural progesterone supplementation can be of great benefit. In the second installment, appearing in next months Nutritional News, Dr. Dean discusses progesterone supplementation and osteoporosis.
Some of the most common symptoms physicians hear from their female patients are problems with weight gain, fatigue, loss of libido, depression, headaches, joint pain and mood swings. Other frequently discovered problems include uterine fibroids, cancer, fibrocystic breast disease, menstrual problems, autoimmune disorders, pre-menopausal bone loss and a high incidence of osteoporosis after menopause. Many physicians and scientists are becoming increasingly aware of a common link between these symptoms and diseases. That common link is often an imbalance between the primary female sex hormones, progesterone and estrogen. (1)
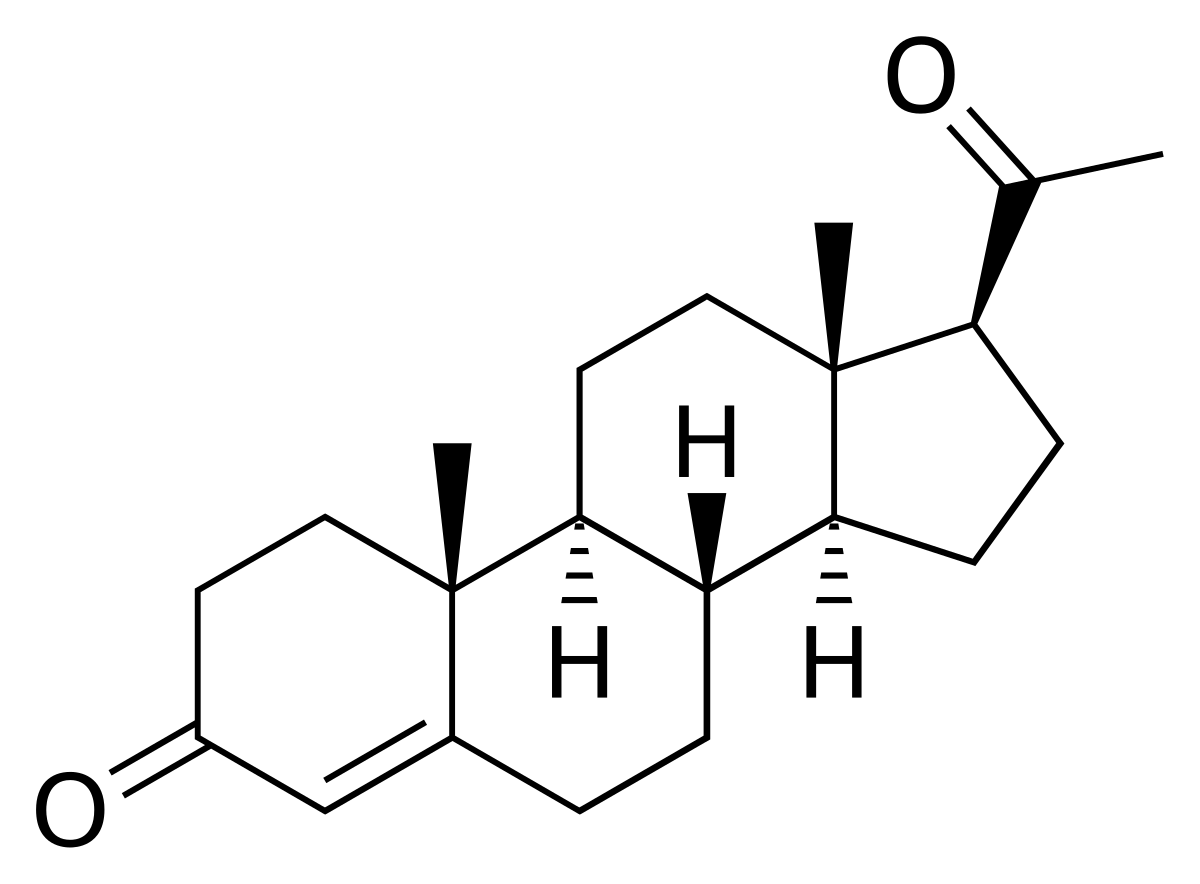
Progesterone and estrogen–along with other steroid hormones like DHEA, pregnenolone, and cortisol–have similar structures Although the structural differences in these hormones may seem minor, these slight differences account for vast differences in their actions. (2,3)
High amounts of estrogen induce a host of metabolic disturbances. Progesterone, on the other hand, has a balancing effect that prevents an excess of estrogen from being toxic and harmful to health.
Progesterone is made in the ovaries of menstruating women and by the placenta during pregnancy. About 20-25 mg of progesterone are produced per day during a womans monthly cycle and up to 300-400 mg are produced daily during pregnancy. Progesterone is a precursor to most steroid hormones and performs a myriad of different functions.
Estrogen regulates the menstrual cycle, promotes cell division, and develops secondary female characteristics during puberty. In non-pregnant, pre-menopausal women, only 100-200 micrograms of estrogen are secreted daily. But during pregnancy, much more is secreted. An important difference between estrogen and progesterone is that high amounts of estrogen are toxic to the body and create a number of harmful side effects. On the other hand, progesterone is free of side effects, even in high amounts. (6,7,8,9)
During the third trimester of pregnancy, women secrete 20 times more progesterone than during the last two weeks of their normal menstrual cycle. Despite the discomfort of carrying excess weight, many women describe that they never felt better in their lives than during the third trimester of their pregnancies! The reason is that the high levels of progesterone at this time produce increased energy and a state of serene well-being. But after delivery, when progesterone production drops suddenly, many women develop postpartum depression due to extremely low levels of progesterone. (10)
Estrogen Dominance – Key to the Puzzle
Unfortunately, most women suffer from a syndrome known as Estrogen Dominance. According to Dr. John Lee, who has pioneered research in this area, estrogen unopposed by progesterone results in a number of adverse effects. These include hypertension, salt and water retention, abnormal blood clotting, excessive body fat, hypothyroidism, painful breasts, fibrocystic breast disease, increased risk of endometrial cancer (cancer of the uterus) and breast cancer.
Estrogen dominance occurs at the age of menopause, when progesterone production falls to approximately 1% of its pre-menopausal level. At this time, the production of estrogen falls to about 50% of its premenopausal levels. This dramatically alters the estrogen: progesterone ratio, causing estrogen to become toxic without progesterone to oppose it. As a result, the risks for breast and uterine cancer, fibrocystic breast disease, ovarian cysts, uterine fibroids, cervical erosions and/or dysplasia, and osteoporosis increase.(11)
Unfortunately, modern orthodox medicine treats menopause primarily with synthetic estrogen.(12) However, the real cause of many menopause-related problems is not a lack of estrogen, but a lack of progesterone. Sadly, many doctors look at menopause entirely as an estrogen deficiency syndrome, and even most pharmacology textbooks state that although levels of estrogen after menopause are too low to support reproduction, they are sufficiently high to maintain support of estrogen-dependent tissues.
The problems of estrogen dominance are not confined to post-menopausal women only. Today, it is extremely common for women to experience recurring menopause-type complaints that begin 10 to 15 years before the time of their menopause (when menstruation ceases). Women as young as thirty years of age often complain of menopause-type problems. This is known as pre-menopause syndrome. (13)
Premenstrual and Pre-menopause Syndromes
In 1931, scientists investigating problems of menstruation identified a group of problems that they labeled premenstrual tension (PMT). PMT was their umbrella term for extreme fatigue, depression, and irritability that many women experienced during the premenstrual period. But as research continued, it became evident that this was part of a syndrome of more than 100 documented symptoms, consequently, the name was changed to premenstrual syndrome (PMS). The most common PMS complaints are weight gain, bloating, irritability, depression, loss of sex drive, fatigue, breast swelling or tenderness, cravings for sweets and headaches.
In 1953, two English physicians Drs. Katharina Dalton and Raymond Greene published the first medical report on PMS. Dr. Dalton observed that injecting progesterone relieved her own menstrual migraine headaches. Dr. Dayton then injected progesterone in other women and found that their PMS was cured.(14,15) Other researchers such as Dr. Joel Hargrove at Vanderbilt went on to show a 90% success rate in relieving PMS symptoms with an oral supplement of progesterone! (16)
The scientists also identified a chronic condition similar to PMS which they called pre-menopause syndrome. They identified two primary causes: [1] anovulatory cycles; and [2] adrenal gland exhaustion. In an anovulatory cycle, a women does not ovulate, and there is no corpus luteum. With no corpus luteum, there is no progesterone secretion. Therefore, women with anovulatory cycles are truly progesterone deficient prior to menopause.(17) Adrenal gland exhaustion from undue stress may also create a progesterone deficiency. As a result of anovulatory cycles and adrenal gland burnout, the problems of estrogen dominance occur early in life in the form of the pre-menopause syndrome.
Progesterone alleviates and prevents both premenstrual and pre-menopause syndromes. Progesterone secretion in women is highest during the two weeks before menstruation. With insufficient progesterone to block the toxic effects of estrogen, PMS is the result. Raising the level of progesterone by supplementation (orally, by injection, or topically) often provides dramatic relief from PMS.(18)
Natural and Synthetic Progesterone
It is important to distinguish between natural progesterone and its synthetic analog, the form most widely prescribed. This synthetic version is not really progesterone at all; it is a progestin. Progestins are synthetic progesterone-like compounds manufactured by pharmaceutical companies. Synthetic progesterones are far more powerful than the bodys own natural progesterone and are metabolized as foreign substances into toxic metabolites. These synthetic progesterones can gravely interfere with the bodys own natural progesterone, create other hormone-related health problems, and further exacerbate estrogen dominance.(19) Side effects of synthetic progesterone include increased risk of cancer, abnormal menstrual flow, nausea, depression, masculinizing effects, and fluid retention.(20,21)
Natural progesterone made from wild yams and soy beans is nearly identical to what the body produces. However, yam-derived natural progesterone should not be confused with yam extracts sold in health food stores. The body easily converts natural progesterone into the identical molecule made by the body.(22) Adverse side effects are very rare.(23) If taken inappropriately, it might slightly alter the timing of the menstrual cycle.
Not All Topical Progesterones are the Same
While I believe that the best way to administer progesterone is topically (transdermally), it can also be taken orally or by injection.(24,25) It should be noted that not all transdermal delivery preparations of progesterone are capable of carrying the hormone through the skin.(24) Adding progesterone to an off-the-shelf moisturizer often results in a product that does not effectively penetrate the skin.
An ideal delivery vehicle is an oil/water emulsion that contains identical components to the fatty tissues of the skin, as well as permeation enhancers and stabilizers in a synergistic balance. The permeation enhancers increase the ability of progesterone to pass the skin barrier.(25,26,27,28) A transdermal progesterone cream should contain at least 400 mg of natural progesterone per ounce. Each one-half teaspoon application would thereby supply a minimum of 26 mg of progesterone. Independent studies reveal that many commercial progesterone creams contain less than 15 mg of progesterone per ounce. In fact, some of these creams contain as little as 2 mg of progesterone per ounce!(29) It should be emphasized that creams that contain only wild yam extract (diosgenin) but no U.S.P. progesterone have absolutely no effect on the level of progesterone in the body.
References:
1. Lipsett, M.P. Steroid hormones, in Reproductive Endocrinology, Physiology, and Clinical Management. Yen, S.S.C., and R.B. Jaffe, eds. Philadelphia: W.B. Saunders Co., 1978
2. Goodman & Gilman.The Pharmacological Basis of Therapeutics. Toronto, MacMillan, 8th edition, chapter 58, 1990.
3. Wills Biochemistry Basis of Medicine. Oxoford, Butterworth-Heinenman Ltd. 1989.
4. Ellison, P.T. et al, The ecological context of human ovarian function. Human Reproduction. 8:2248-58, 1993.
5. Hileman, Beth. Reproductive estrogens linked to reproductive abnormalities, cancer. Chemical and Engineering News, January 31: 19-23, 1994.
6. Op cit, Goodman and Gillman, The Pharmacological Basis of Therapeutics.
7. Op cit, Steroid hormones, in Reproductive Endocrinology, Physiology, and Clinical Management.
8. Elks, Peripheral effects of steroid hormones, implications for patient management, JAMWA. 48:41-55, 1993.
9. Textbook of Clinical Chemistry, Tietz, ed. Philadelphia, Sanders, 1986.
10. Harris, B., Maternity blues and major endocrine changes. Brit. Med. Jour. 308:949-53, 1994.
11. Lee, John R., What Your Doctor May Not Tell You About Menopause . Warner Books, May, 1996.
12.Gambrell, R.D. The menopause: benefits and risks of estrogen-progestogen replacement therapy. Fertil Steril, 37:457-74,1982.
13. Neugarten, B.L., Menopuase symptoms in woman of various ages. Psycom Med. 27-266-73, 1964.
14.Dalton, K. The Premenstrual Syndrome and Progesterone Therapy, Chicago, Year Book Medical Publishers. 1977.
15. Dalton, K. Once a Month, Pomona, CA, Hunter. 1979.
16. Hargrove, J.T., W.S. Maxson, A.C. Wentz, and L.S. Burnett. Menopausal hormone replacement therapy with continuous daily oral micronized estradiol and progesterone. Obstetrics & Gynecology. 71:606-12, 1989.
17. Campbell, B.C., and P.T. Ellison. Menstrual variation in salivary testosterone among regularly cycling women. Horm Re,s 37:132-36, 1992.
18. Op cit , Lee, John R., What Your Doctor May Not Tell You About Menopause.
19. Edgren, RA Clinical Use of sex hormones, Year Book Medical Publications, 1980.
20 Physicians Desk Reference (PDR), Montvale, N.J. Medical Economics Data, 1995.
21 Bergkvist, L., H.O. Adami, I. Persson, R. Hoover, and C. Schairer. .The risk of breast cancer after estrogen and estrogen-progestin replacement. New England Journal of Medicine, 321:293-97.1989
22. Op cit, Hargrove, J.T., W.S. Maxson, A.C. Wentz, and L.S. Burnett. Menopausal hormone replacement therapy with continuous daily oral micronized estradiol and progesterone
23 Ottoson, U.B., B.G. Johansson, and B. von Schoultz. Subtractions of high -density lipoprotein cholesterol during estrogen replacement therapy: a comparison between progestogens and natural progesterone.American Journal of Obstetrics and Gynecology, 151:746-50, 1985.
24. Johnson, Blankenschtein and Langer, Permeation of Steroids Through Human Skin. Journal ofPharmaceutical Sciences, Vol. 84, No. 9, Sept. 1995. Pages 1144-1146, 1995.
25 Hadgraft, J. and Guy, R.H. Transdermal Drug Delivery, Volume 35, Drugs and the Pharmaceutical Sciences Marcel Dekker, 1989.
26. Chien, Y.W. Novel Drug Delivery Systems. 2nd Ed., Drugs and the Phannaceutical Sciences Volume 50, Maccel Dekker, 1992.
27. Waiters, K.A. Penetration enhancers and their use in Transdermal Therapeutic Systems, in Transdermal Drug Delivery, Volume 35, Drugs and the Pharmaceutical Sciences Marcel Dekker, 1989.
28. Barry, B.W. Dermatological Formulations. Percutaneous Absorption. Drugs and the Pharmaceutical Sciences Volume 18, Marcel Dekker, 1983.
29. Range of Progesterone Content of Body Creams & Oils prepared by Aeron Lifeycles in Lee, John R., What Your Doctor May Not Tell You About Menopause . Warner Books, May, 1996.